Abstract
Graft-versus-host disease (GVHD) is the one of the most serious complications of the allogenic stem cell transplantation (SCT). Especially, chronic GVHD has complex pathologies including the aspects of autoimmune diseases and microangiopathies. Recombinant thrombomoduin (rTM), which shows anticoagulant activity independent of antithrombin through binding to thrombin to activate protein C, has been used for disseminated intravascular coagulation (DIC). Recent studies have also demonstrated that rTM suppresses inflammatory response through various pathways including activated protein C (APC), degradation of HMGB1, inhibiting inflammatory cytokine and increasing regulatory T-cells (Treg), leading to attenuate tissue damages in animal models such as acute respiratory distress syndrome and liver injury by heatstroke. In acute GVHD mice model, rTM is reported to have therapeutic effect with contribution of Treg and blockade of HMGB1. In addition, rTM protects endothelial cells from calcineurin inhibitor-induced cytotoxicity in vitro using human umbilical vein endothelial cells. Thus, rTM is expected to show beneficial effects for post transplant complications. Actually, rTM has been sometimes used for severe veno-occlusive disease, DIC and thrombotic microangiopathy after SCT in clinical settings, but it is not clear whether rTM could have impact on acute or chronic GVHD themselves. In this study, we investigated the role of rTM especially focusing on preventing chronic GVHD in a rodent model.
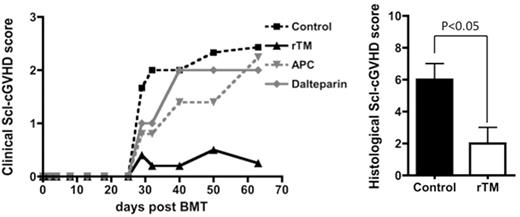
Bone marrow and splenocyte from donor mice (B10.D2) were transplanted into irradiated host mice (Balb/c) to induce sclerodermatous chronic GVHD (Scl-cGVHD). First, to demonstrate whether rTM could ameliorate the Scl-cGVHD, irradiated host mice were given splenocytes with rTM. Compared with the control group, rTM significantly improved chronic skin GVHD. However, rTM did not improve survival rate when increased dose of splenocytes was given to induce lethal intestinal GVHD together with Scl-cGVHD. In addition using another mice strain combination mimicking acute GVHD, rTM did not show any impact on ameliorating GVHD. Collectively, these results suggested that rTM had a beneficial effect on skin sclerodermatous lesions, not systemically. Next, to test whether rTM has therapeutic effects against skin lesions, rTM was started from 3 weeks after transplantation when Scl-cGVHD had already appeared. rTM did not improved Scl-cGVHD anymore. Next, to clarify whether the prophylactic mechanism of rTM to Scl-cGVHD is due to anticoagulant activity alone and/or complicated immure regulations by APC and rTM, Scl-GVHD mice was given dalteparin, APC and rTM, respectively. As shown in figure below, only rTM attenuated Scl-cGVHD with retaining normal skin structure and less inflammatory cell invasion compared to other groups, suggesting that rTM related immune regulation was a significant contributor to skin prophylactic effect, not anticoagulant activity. Though skin lesions were dramatically different among groups, in splenocytes there were no significant difference of cell subpopulation, T-cell activation and inflammatory cytokines (TNFα, IFNγ, IL17A). There was also no significant difference in regulatory B-cell, which was known to have a suppressive role in Scl-cGVHD model, and Treg. Moreover to confirm that rTM dose not influence these properties in vivo and in vitro, we analyzed splenocytes after repetitive administration of rTM to non-treated mice and short-term culture of splenocytes mixed with rTM. As expected, there was no significant difference by adding rTM in cell subpopulation including Treg, Breg and cytokine production in vivo and in vitro. From these findings, prophylactic mechanism of rTM in Scl-cGVHD was not due to anticoagulant activity nor APC related anti-inflammatory effects, but more likely to rTM related immune regulation. HMGB1 is one of the targets that rTM acts on as an immune modulator, but a previous report demonstrated that HMGB1 blockade attenuated GVHD systemically including skin, intestine and liver. In contrast to our findings that rTM worked mainly at skin lesions, unknown mechanisms of immune regulation by rTM might exist. In conclusion, rTM would be a promising drug for preventing sclerodermatous skin GVHD in addition to improving various complications associated with coagulation abnormalities.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal